Join NYC Cognitive Therapy’s Upcoming Therapy Groups
Posted: August 4, 2022 Filed under: All Leave a comment |
| Mindfulness & Mental Health Group NYC Cognitive Therapy is offering a virtual 12-week Mindfulness & Mental Health Group led by Gianna LaLota, MHC-LP and Katie Zaborsky. This group is suited for both beginners who are new to mindfulness and meditation, as well as, individuals who are looking to deepen their practices. This 12-week closed group will consist of 10-12 group members (ages 18 and up) who are looking to learn more about mindfulness and mental health in a supportive group setting. Mindfulness has been clinically proven to reduce feelings of stress, depression, and anxiety by helping individuals cultivate greater present-moment awareness, as well as, compassion for themselves and others. Not only will group members leave the group with a greater understanding of basic mindfulness principles, they will also be equipped with various techniques and tools that they can implement in their daily lives. The group will meet via Zoom on Monday evenings from 7:15-8:30pm starting sometime in mid-late September. Please email gianna@nyccognitivetherapy.com for more information. This group covers: -Session 1: Introduction to Mindfulness -Session 2: Mindfulness of the Breath -Session 3: Mindfulness of Emotions -Session 4: Mindfulness of Thoughts -Session 5: Mindfulness of the Body -Session 6: Mindful Movement Practice -Session 7: Mindfulness in Your Daily Life -Session 8: Mindfulness for Self-Compassion -Session 9: Mindfulness and Acceptance -Session 10: Engaging Your 5 Senses & Grounding -Session 11: Mindfulness for Focus & Increased Performance -Session 12: Summary & Wrap-Up |
| CBT Skills Group for Social Anxiety NYC Cognitive Therapy is also offering a virtual 15-week CBT Skills Group for Social Anxiety led by Gianna LaLota, MHC-LP and Jessica Nathanson. Cognitive Behavioral Therapy can be effectively utilized to help individuals struggling with social anxiety to reduce their anxiety in social settings, academic settings, career settings, etc. The 15-week closed group will also contain 10-12 members (ages 18 and up) whose primary concern is social anxiety. The goal of the group is to help members address concerns, including socializing, making friends, dating, increasing assertiveness and communication skills, advancing one’s career, overcoming the fear of public speaking, and other performance-related anxiety using CBT skills and techniques. The group will meet via Zoom on Tuesday evenings from 6:30-8:00pm starting sometime in mid-late September. Please email gianna@nyccognitivetherapy.com to learn more. This group covers: -How to challenge anxious thoughts and develop more balanced thinking -Creating a fear hierarchy -In-session exposure exercises and behavioral experiments -Assertiveness training -Tips for small talk and having group conversations -Techniques for combating rumination -Attention training and mindfulness for anxiety |
| Don’t take our word for it. Hear what current group members have to say: “The group has been helpful for tackling my social anxiety triggers, and I have learned new strategies to use in the future, as well. I have made some great progress each week, due to having accountability and structure. The pandemic is such a strange time, with some new social anxiety triggers, so I think the group has been good in helping me feel like I’m not regressing with my social coping skills. It is also relieving to be able to talk about social anxiety publicly, something I have never done before, but that normalizes feeling awkward at times.”- C.D., group member -“The group therapy for social anxiety has been extremely helpful for me in learning about and developing the tools needed to manage, and hopefully overcome, my social anxiety. This is a problem that has plagued me for much of my life, and the social anxiety group offered the structure and supportive learning environment needed to help overcome some of the issues I face day-to-day. Gianna is a very professional, compassionate, and innovative facilitator, and the group members are highly supportive. It has been helpful also to find through the group setting that I am not alone in experiencing social anxiety issues. For anyone experiencing ongoing social anxiety, and wanting to work on managing it, I would highly recommend this group.”- M.P., group member -“I have found this group very helpful for confronting my social anxiety – from useful exercises rooted in CBT, to intra-group exposures to hearing from others with similar experiences – I would certainly recommend it to others.”- J.P., group member |
Improve your love relationship by talking about sex
Posted: November 3, 2018 Filed under: All Leave a comment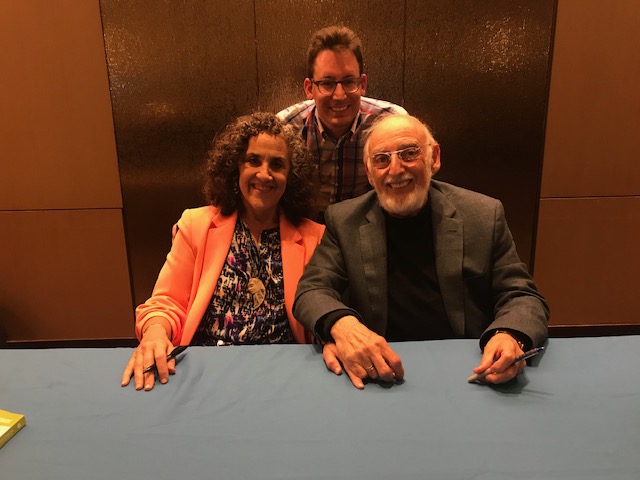
Noah Clyman LCSW-R & Drs. Julie & John Gottman
I recently had the pleasure of attending a 3 day workshop with couples’ therapy experts Drs. Julie & John Gottman who are world renowned for their work on marital stability and divorce predictions. You may recognize them as the authors of the New York Times bestseller, The Seven Principles for Making Marriage Work: A Practical Guide from the Country’s Foremost Relationship Expert. I learned their innovative theory about how to make relationships work, along with research based skills for a great sex life, improving friendship, and resolving conflict. There are so many pearls of wisdom and this blog post will touch on the importance of talking about sex.
According to Drs. Gottman, there is no more stable and replicated result in the sex field than this: being able to talk comfortably about sex is strong related to satisfaction. Not just with sex, but with the whole relationship. And the results are not weak, they are dramatic. Quantity as well as the quality of the talking about sex, are strongly correlated with a couples’ happiness. Statistically speaking, only 9% of couples who can’t comfortably talk with one another about sex say that they are satisfied sexually, as well as satisfied in general with their relationships. On the other hand, over 50% of couples who can (and do) talk with one another openly about sex are satisfied sexually and are satisfied in general with their relationships. That’s a difference of forty-one percent! Amazing.
Research on sexuality strongly points to the importance of being able to talk intimately with one’s partner to enhance the quality of sex in your relationship. Yet having these conversations is very difficult for American couples from an African, Anglo-Saxon, or East European cultural background. Drs. Gottman–who have been analyzing videotapes of couples talking about their sex life in their “Love Lab” for decades–found that most couples have a great deal of trouble being clear and specific about what they want and don’t want in the bedroom. There’s an enormous fear of rejection which comes from a lack of trust and openness with each other.
Interestingly, this isn’t true of many heterosexual couples who are Latino and haven’t been made to feel guilty by strict religion. In some ways, these cultures support direct and frank non-defensive conversations with one’s partner about sex, romance, and passion. (This is not to say that all Latino couples are comfortable talking about sex. Many are not). Drs. Gottman discovered these facts about Latino cultures in America during a national survey they designed for Readers Digest. They also found that the same was true of gay and lesbian committed couples, in a 12-year study they did with Robert Levenson. Generally, Latino and same-sex couples didn’t make assumptions about eroticism. They considered it their responsibility as lovers to know what their partner did and didn’t find erotic.
To facilitate the process of conversation about sex, romance, and passion for couples who may feel uncomfortable with these intimate topics, it is important for couples to learn how to how their partner basic questions about sexual preferences, and then remember the answers. Remember: if you know your partner’s preferences, you will be able to create more excitement and pleasure for your partner. I look forward to helping couples improve their relationships from resolving conflict, to deepening friendship, to having great sex.
8 tools to defeat your ‘workaholic’ ways
Posted: August 4, 2018 Filed under: All Leave a comment
I am a workaholic. While on vacation last week, I became cognizant of the benefits of r&r and was inspired to write a blog that might help my fellow workaholics to address this issue. Do you find it difficult to disengage from work? An imbalance between your work life and your personal life may be behind of myriad of other problems, such as anxiety, depression, or insomnia. Are you obsessed with working to the exclusion of other things in your life? Some people work as though they were addicted to working. Have you convinced yourself that you have to work harder than everyone else? At your place of work, are you always the first to arrive and the last to leave? Has anyone ever accused you of being a workaholic or a perfectionist? Do you feel as if you are addicted to work? Work and your professional identity may be overly tied to your self-esteem so that you over-allocate time to work pursuits. Do you feel badly about yourself when you are not doing work? Do you view non-work activities as a waste of time? Do you believe that any idle time should be filled with some useful activity towards a goal? Have you come to devalue activities done for the sake of leisure or rest? If so, here are some cognitive and behavioral therapy techniques for you to try:
- Ask yourself, Why am I the exception to the rule that human beings need rest and relaxation? In other words, challenge the idea that you do not require rest or pleasure in your life—all human beings do.
- Imagine what would happen at work if you were incapacitated in some way. Would the business cease to exist, or would it find some way to make up for your absence? Challenge your tendency to overestimate your importance at work. Paradoxically, people who take breaks and recharge are often more productive at work.
- Experiment with putting some rest and pleasure into your life and taking away some of the time currently allotted to work. For example, if you are working more than eight hours a day, commit to leaving work at an earlier time this week. Spend extra time doing something enjoyable.
- Shorten your to-do list this week to essentials only.
- In your own personal currency (i.e., in your mind), consider increasing the value of moments of pleasure and decreasing the value of accomplishments.
- Create a “Buffer zone:” about an hour before getting ready for bed, begin to transition away from your “active self” by restricting your activities to those that are relaxing and enjoyable to you.
- Say no to at least one request this week.
- Think of the needs of people who currently depend on you. Now think of your own needs. Is your list of needs shorter? If so, why? How are your needs different from theirs? Why are you an exception? What is missing from your list of needs? Add to your list of needs and make time to de-stress and unwind every single day.
In summary, like any other human being, you need time for rest and relaxation. Far from being wasted time, making a conscious and consistent investment in “self-care” will help you be happier, more self-aware, calmer, and more productive throughout your days.
Online Hair Loss Study
Posted: May 25, 2018 Filed under: All Leave a comment
|
|
|
|
|
|
|
|
https://sites.google.com/view/myhairlossstudy
MEDITATION 101
Posted: May 7, 2018 Filed under: All Leave a comment
Author: NYC-NYC staff therapist, Mike Comparetto, LMSW.
CBT Therapists have lots of tools to teach our clients. But I often think, what if I had to pick just one to share with people? My answer, without hesitation, would be mindfulness meditation. It is the most powerful and transformative tool that I have ever come across, and these days we have ample studies to prove it. If you are a skeptic (as you should be), just Google “medical research on meditation” and you will find results from Harvard Medical School, Time Magazine, Mayo Clinic, the CDC, etc. showing a vast array of benefits both mental and physical. Here is just one article from the APA listing many of them.
What is Meditation?
This question is simultaneously very simple and very complex. Let’s start with the simple, and we can save the complex discussions for another day. There are many types of meditation, but for this article I will only be referring to Mindfulness Meditation. The officially accepted definition of mindfulness, penned by Jon Kabat-Zinn, is “…awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally.” Mindfulness can be practiced while doing just about anything, but when we say meditation, this usually refers to practicing mindfulness in a seated position. There are ways to do walking meditation, standing meditation, and other forms of moving meditation, but seated meditation is the most common, and that’s what we will be focusing on here.
What is the Aim of Meditation?
If I could boil the aim of meditation down to one thing, it would be switching our frame of mind from conceptual to experiential. Meditation allows us to tap in to our lived experience, and let go of the stories we tell ourselves about it. These stories often magnify (or in some cases manufacture) the pain and difficulty in our lives. Mindfulness also reminds us that we never have to endure our experience for more than one moment at a time, which is quite freeing. All experiences are impermanent, and meditation brings this into direct focus.
If you learn how to effectively manage your mind, your thoughts and actions start to lead you away from suffering and towards happiness. This is why we practice meditation- to end suffering.
“Mindfulness helps us get better at seeing the difference between what’s happening and the stories we tell ourselves about what’s happening, stories that get in the way of direct experience. Often such stories treat a fleeting state of mind as if it were our entire and permanent self.” –Sharon Salzberg
How to Meditate
There are so many different ways to meditate that it can be overwhelming. A Google search on “how to meditate” returns 258,000,000 results. I think when you are starting out, it is important to just find a style that is accessible to you and do it. Later on, if you find that that particular style or tradition doesn’t really resonate with you, you can do your research and find the one that does. In the beginning though, any meditation is better than no meditation.
Since this article is about the bare basics, let’s establish some guidelines for just about all types of meditation:
1) Meditating for 5 minutes every day is better than meditating for 1 hour once a week. Developing the discipline to cultivate a daily practice is extremely important, and doing it every day creates the momentum needed to get results. If that means starting with only 5 minutes, then do what you can.
2) Try not to judge your meditation. You may have some meditations that leave you feeling great, some that leave you feeling tired, discouraged, or indifferent. They are all equally valuable. Nobody is bad at meditation- it is a constant practice. Each time you redirect your mind, you are building new neural pathways in your brain.
3) Don’t seek out particular states of mind or experiences. As a beginning meditator, you will most likely not have the ability to sit down and immediately cultivate the exact mind-state you are looking for (if you can, let me know your secret!). Meditation is about observing what is arising in the present moment- it is not about creating an alternate reality to dwell in. Remember that mindfulness is meant to cultivate a non-judgemental mind. That is absolutely critical. The goal of meditation (you will not always achieve this goal and that’s ok) is to meet each moment without adding your own commentary, opinion, interpretation, or sense of like or dislike to it. Yes, it’s as hard as it sounds, but that’s why we call it a meditation practice.
4) Have compassion for yourself. You will quickly find that the mind can sometimes be, well, kind of a jerk. The last thing you ever want to do is make things worse by beating yourself up when you can’t focus for more than half a second, or when your mind won’t stop repeating the same thoughts over and over. This is all a part of meditating, and even advanced meditators experience a mind that is uncooperative at times. It’s all about how you relate to those experiences. Try to use it as an opportunity to observe what it’s like to be in a busy mind (or an angry mind, a sad mind, etc).
5) Develop patience. I don’t know how to break this to you, but you are not going to achieve enlightenment after your first meditation. You will most likely see some immediate results, but the real benefits come weeks, months, years, and decades into the practice. As a bonus, you can use your meditation to observe the mind’s compulsion to want instant gratification.
6) Don’t worry what anyone thinks about it. If your friends think you are weird for meditating, or you fear that your co-workers will never speak to you again, just let it go. Nothing is more important than finding true peace and happiness. Be yourself, be free, and do what makes you happy.
Keeping those guidelines in mind, use the resources I have provided at the end of this blog to try meditation. If you are absolutely brand new to meditation I suggest starting with the Headspace app, or this guided meditation.
I hope meditation can be as powerful and transformative for you as it has been, and continues to be, for me. Supposedly the last words the Buddha ever spoke were, “Strive on with diligence.” May you strive on towards liberation and well-being.
-Mike
Resources
Get in touch with us to book a session:
Apps:
Webpages:
Kristin Neff – Self Compassion Exercises
Tara Brach – Guided Meditations
Books:
Meditation for Beginners – Jack Kornfield
How to Meditate – Pema Chodron
Real Happiness: The Power of Meditation – Sharon Salzberg
Against the Stream – Noah Levine
Got Clutter?
Posted: November 7, 2017 Filed under: All 1 Comment
NEW: Behavioral Activation for Depression, and CBT-i for Insomnia
Posted: September 26, 2017 Filed under: All Leave a comment
At NYC Cognitive Therapy, our staff are trained in two NEW and HIGHLY EFFECTIVE short-term treatments: Behavioral Activation for Depression and CBT-i for Insomnia.
To schedule an appointment, call 347-470-8870, or email us at info@nyccognitivetherapy.com.
BEHAVIORAL ACTIVATION WHAT IS IT:
A powerful, empowering, and highy effective treatment for those suffering from major depression and other forms of depression. Behavioral Activation (BA) works by helping clients reengage in those aspects of their lives that bring the greatest meaning and pleasure.
WHY DO IT:
BA is a proven and powerful behavioral approach that is often more effective in treating major depression than use of anti-depressant medications, and is one of the most powerful psychosocial treatments available today.
WHEN DO IT:
Ask your therapist about BA if you score mild, moderate, or severe on a depression inventory. Click here to find out Am I depressed?
To schedule an appointment, call 347-470-8870, or email us at info@nyccognitivetherapy.com.
COGNITIVE BEHAVIORAL THERAPY FOR INSOMNIA (CBT-I)
WHAT IS IT:
CBT-I is an effective treatment for chronic sleep problems. It is as effective as sleep medication in the short term and more reliable and durable than medications in the long term. CBT-I includes strategies to retrain the body to sleep, reduce factors interfering with sleep, and increase sleep drive to resume the body’s natural rhythms.
WHY DO IT:
Evidence suggests insomnia is an important target in improving overall mental health. Improves sleep in 70-80% of patients.
WHEN DO IT:
Ask your therapist about CBT-I if you have been experiencing sleep problems for at least one month.
To schedule an appointment, call 347-470-8870, or email us at info@nyccognitivetherapy.com.
Got Healthy Habits?
Posted: July 26, 2017 Filed under: All 1 Comment
Often, we have the capability for a desired behavior -we can do (or keep ourselves from doing) a behavior if given optimal circumstances. But we can’t get it to happen reliably in all relevant contexts.
As therapists, when we see that a behavior isn’t reliably happening in all needed contexts, we default to assuming the problem is not enough motivation and intervene to strengthen motivation. Rather than rely solely on motivation, you can DESIGN and BUILD behavior change with scheduled baby steps. I’ve been working to strengthen this core competency by playing with tiny habits and habit-stacking to support my own and my client’s behavior change.
If this is interesting to you, try a week-long experiment with tiny habits. BJ Fogg, a researcher at Stanford, gives away his method in a super helpful bite-by-bite way (and it’s free!). You can go to this link and register for the next Tiny Habits Session http://www.tinyhabitsacademy.org/
In brief, a “Tiny Habit” is a behavior —
- you do at least once a day
- that takes you less than 30 seconds
- that requires little effort
You use an already established anchor, something you already nearly always do, a well-established habit. After I _[anchor]__, I will [tiny habit].
To get the hang of the tiny habit steps, I started with the easiest set I could think of (that still were important to me). For example:
After I start the coffee, I will:
1. drink a glass of water
2. take a vitamin
3. mindfully notice the present moment using all my senses
After 2 weeks, I’ve found that all the above are regularly happening and I am kind of smitten with how fun this is.
I also invite you to check out two exciting offerings that will be coming up (see below for details). Space in both is limited, so definitely contact us NOW to get your spot. Thanks!
–Noah Clyman, LCSW-R, ACT
TEAM therapy: Brief Intensive Preview Video! — Feeling Good
Posted: July 26, 2017 Filed under: All Leave a commentRegister now! The San Francisco summer intensive is right around the corner!
via Brief Intensive Preview Video! — Feeling Good
New @ NYCCT: COGNITIVE BEHAVIORAL THERAPY FOR INSOMNIA
Posted: May 6, 2017 Filed under: All Leave a comment
Noah Clyman, LCSW-R of NYC Cognitive Therapy has completed CBT-I training and demonstrated proficiency in the CBT-I program that was developed by Dr. Greg D. Jacobs and tested at Harvard Medical School.
COGNITIVE BEHAVIORAL THERAPY FOR INSOMNIA
Over 50% of adults now complain of difficulty sleeping, half of these chronically. We now know that sleeping pills are not the solution to insomnia and that it is possible to successfully treat insomnia using cognitive-behavioral therapy (CBT). CBT has been endorsed by the National Institutes of Health as an effective and preferred method for treating insomnia.
Research on CBT shows the following:
* 75% of insomnia patients experience significantly improved sleep
* The majority become normal sleepers
* 85- 90% reduce or eliminate sleeping pills
* CBT is more effective than sleeping pills
Did you know? Sleeping pills fail to treat the causes of insomnia, which are thoughts and behaviors. By treating only insomnia’s symptoms, any improvement in sleep can only be temporary, thereby perpetuating the cycle of insomnia and sleeping pills. This cycle can become a trap that can lead to dependency. Many patients are aware of the drawbacks of sleeping pills and prefer non-drug approaches to managing insomnia but don’t know how to escape their reliance on sleeping pills. Even if the ideal sleeping pill were developed-one that had no side effects and that produced natural sleep-it would still reinforce the belief that the cure for insomnia comes from something external; and, it wouldn’t treat the causes of insomnia, which are thoughts and behaviors. So sleep may improve while taking a sleeping pill, but as the pill is stopped insomnia usually returns.
Did you know? The success of CBT is based on a central theme: insomnia can only be treated by addressing all of the underlying causes. In most instances, the causes of insomnia are thoughts (cognitions) and behaviors (habits) which are learned and can be unlearned. Some examples include:
*negative, distorted thoughts and beliefs about insomnia,
*feeling of loss of control over sleep,
*inadequate exercise or exposure to sunlight,
*going to bed too early or sleeping too late,
*trying to control sleep rather than letting it happen,
*lying awake in bed, frustrated and tense.
5 Sleep Behavioral Skills to DRAMATICALLY Improve Sleep
- Establish a regular arising time: To promote a regular arising time, pair it with a pleasurable activity: walk the dog, read the newspaper, exercise or take a morning walk, etc. By establishing a consistent arising time, you will fall asleep and stay asleep more easily, and sleep more deeply. This will improve sleep efficiency and make the bed a stronger cue for sleep.
- Establish a relaxing wind-down routine during the hour before bed (reading, “neutral” television, or a hobby as opposed to problem solving, computer work, finances, work-related activities, phone calls, “negative” tv). However, don’t become so sedentary during the wind-down period that drowsiness occurs. Use physical activity and light to ward off fatigue and drowsiness and don’t be a “couch potato.” Avoid computers the hour before bed and during the night since the light exposure may promote wakefulness.
- Break habits that make the bed a cue for wakefulness. Poor sleepers have often lain awake for so many nights that the bed and bedroom have become strong cues for sleeplessness! As a result, just getting into bed triggers a learned arousal response and wakefulness. In fact, it is not uncommon for insomniacs to find themselves falling asleep in front of the television in the living room, yet when they get into their bed to go to sleep, they become wide awake because the bed has become such a strong cue for wakefulness.
- Develop habits to associate the bed with drowsiness: Practice identifying the internal cues for drowsiness (eyelids dropping, head nodding, yawning, reading the same line in a book several times) rather than relying on external cues such as the clock, a bed partner’s bedtime or the end of the evening news.
- Follow the half hour-half hour rule. If patients don’t fall asleep within 20 or 30 minutes, or if they awaken during the night and don’t fall back asleep within 20-30 minutes, they should not lie in bed tossing and turning (since focusing on the clock only heightens anxiety about falling asleep, the 20-30 minute limit should be estimated). Instead, they can go into another room and engage in a quiet, relaxing activity such as watching television, reading a book, magazine, or catalog until drowsy, then attempt to go to sleep again.
7 Lifestyle Considerations to DRAMATICALLY Improve Sleep
- Alcohol: suppresses deep sleep and dream sleep and exacerbates snoring. Alcohol in the evening should be limited to two drinks and not after 7 pm.
- Caffeine: disrupts sleep because it produces stimulant effects (faster brain waves, heart rate, etc.) that can persist for up to eight hours in sensitive people. Caffeine should not be consumed after 3:00 pm; total daytime use should be limited to two cups.
- The Food-Sleep Connection: Those who desire to fall asleep more easily should eat a high carbohydrate snack and avoid high protein foods the hour or two before bedtime. Those who desire to minimize nighttime awakenings should eat a carbohydrate snack immediately before bedtime, which will increase serotonin levels during the night and help one stay asleep. Having a light carbohydrate snack before bedtime will also ensure that sleep isn’t disturbed due to hunger.
- Role of exercise: Moderate physical activity (lawn work, taking stairs instead of elevators, walking) and vigorous aerobic activity improve sleep by promoting greater rise and fall in body temperature that persists for up to five hours. This greater rise and fall in temperature can make it easier to fall asleep and stay asleep. The beneficial effect of exercise is greatest when exercise occurs within three to six hours of bedtime. Try to engage in 20-30 minutes of physical activity at least every other day to improve sleep.
- Room temperature: A cooler room will improve sleep by producing a drop in body temperature. In constrast, a warm room will inhibit the drop in body temperature and impair sleep. (Have a spouse or bed partner use an extra blanket if they prefer a warmer room).
- Baths: A hot bath before bed will improve sleep. Must be kept hot for 25 minutes and should be taken about two hours before bedtime. (A great way to relax and a good substitute on days when you can’t exercise).
- Noise: White noise (the sound of a fan, air conditioner, or commercial white noise machine) masks noise, is relaxing to the brain, and can make it easier to fall and stay asleep.
CBT COMPONENTS
Techniques taught in CBT include:
* changing sleep thoughts and behaviors
* lifestyle habits that improve sleep
* relaxation techniques
WHO WOULD BENEFIT
* individuals with problems falling asleep or waking during the night
* individuals who wish to reduce or eliminate sleep medications
To Get Started Using Powerful CBT Methods to Conquer Your Insomnia, Call us at 347-470-8870, email info@nyccognitivetherapy.com, or visit our website, NYC Cognitive Therapy.




